Description
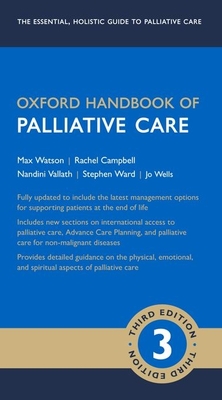
The Oxford Handbook of Palliative Care returns for a third edition, maintaining the concise yet comprehensive format suited to the busy practitioner for quick access to key information, and fully updated to reflect changes in the palliative care landscape.
Featuring an increased emphasis on non-malignant diseases such as dementia, this authoritative text combines evidence-based care with the bedside experience of experienced palliative care professionals to give the reader a complete overview of the physical, emotional, and spiritual aspects of care for the end-of-life patient. Symptom management is covered in detail, with updated formulary tables and syringe driver protocols, and a new chapter on international perspectives to broaden the reader's perception of methods for delivering end-of-life care.
The third edition of the Oxford Handbook of Palliative Care is the essential companion for all of those working with adults, children, and families with palliative care needs, in both hospital and community settings.
The following correction has been made online and will be included in the first reprint. Readers can get in touch with us directly using the contact details on the back of the book or at our online form via the address below with questions or comments: https: //global.oup.com/academic/category/medicine-and-health
Chapter 5. Page 109
The dose for Hyoscine butylbromide sc has been amended in line with NICE guidance (https: //bnf.nice.org.uk/drug/hyoscine-butylbromide.html): '20-120 mg 4 hourly' has been corrected to '20-80mg 4 hourly'.
About the Author
Max Watson, Director Project ECHO Hospice UK, London; Consultantin in Palliative Medicine, Western Trust, Enniskillen; Visiting Professor, University of Ulster, Belfast, UK, Stephen Ward, Teacher Practitioner Pharmacist, Belfast Health and Social Care Trust, Belfast, Northern Ireland, Nandini Vallath, Academic Consultant, Palliative Care Training Program Coordinator for India, Indo-American Cancer Association, Houston, USA, Jo Wells, Nurse Consultant (Triage), Southern Adelaide Palliative Service, Australia, Rachel Campbell, ADEPT Clinical Leadership Fellow and Speciality Trainee in Palliative Medicine, Northern Ireland Medical and Dental Training Agency, Northern Ireland, UK Max Watson is Director of Project ECHO at Hospice UK in London, former Medical Director of Northern Ireland Hospice, and Honorary Senior Lecturer at Queens University Belfast. Max is an author and editor with OUP including the End of Life Care series. His research interests include generalist palliative care education, cancer cachexia, dementia care at the end of life, and the use of bedside ultrasound. Trained in theology and medicine, Max worked in Nepal as a GP before palliative training in London and Belfast. He has developed a range of teaching programmes for generalists, including the European Certificate in Essential Palliative Care, used in the UK, India, Malta, Nepal and Kyrgystan.Since 2014 he has been pioneering Project ECHO methodology as a means of democratising medical knowledge, tele-mentoring and building communities of practice.Clinically, Max currently provides a Palliative Medicine Liaison service to acute hospitals in the Western Trust in Northern Ireland. Rachel Campbell is a speciality trainee in palliative medicine at the Northern Ireland Medical and Dental Training Agency (NIMDTA), and was formerly was an ADEPT Fellow on the Clinical Leadership Fellow's Program. Nandini Vallath is a clinical consultant and director of projects at the Trivandum Institute of Palliative Sciences in India. She was awarded the 2015 Cancer Aid Society Palliative Care Award for Excellence and Leadership in the SAARC region. Nandini collaborates with NGOs and government officials to develop policies to improve palliative care, and has helped develop modules for palliative care at undergratudate ad professional levels. Stephen Ward is a Teacher Practitioner Pharmacist in the Belfast Health and Social Care Trust. In addition to providing a clinical pharmacy service in the Royal Victoria Hospital, he has also developed a medication safety programme for final year medical students. Stephen studied pharmacy in Queen's University Belfast before working as a hospital pharmacist in Uganda. Following this, he worked as a clinical pharmacist in the Belfast Trust and Northern Ireland Hospice. His research interests include medical education, palliative care and respiratory medicine. Jo Wells is a Nurse Consultant at the Southern Adelaide Palliative Service in Australia, and was formerly a Support Services Co-ordinator at The Leukaemia Foundation, South Australia.